Portosystemic Encephalopathy in a Dog- Juniper Publishers
Journal of Dairy & Veterinary Sciences- Juniper Publishers
Abstract
Portosystemic shunt is an abnormal vascular
connection between the portal and systemic venous system. Due to this
abnormal network of vessels, portal venous blood and its toxic
by-products by-pass the liver and directly mix into the systemic
circulation. It is a well-known congenital cause of encephalopathy which
is characterized by high ammonium levels. Our case; a two-year-old male
dog was brought to our clinic with tonic-clonic epileptic seizures and
allotriophagia presenting for the last four months.Diagnosis of
portosystemic shunt was made, and a surgical operation was planned.
After the operation, ammonium levels decreased sharply. However,
ammonium levels have started to rise again the month following the
procedure and leaded to more severe symptoms. Consequently, the patient
was euthanized after three months.
Keywords: Portosystemic shunt; Encephalopathy; Hepatic encephalopathy
Introduction
Portosystemic shunt is an abnormal venous connection
between the portal system and systemic circulation; this alternative
route causes by-passing of blood and its toxic metabolites through the
liver and directly drain into the systemic venous circulation. Many
different types of congenital port vascular anomalies have been reported
in dogs [1]. The incidence of congenital portosystemic shunt has been
reported as 0.18% of in dogs[2]. Extrahepatic portosystemic shunts are
usually seen in small-breed dogs. Affected dogs generally show symptoms
before the age of two, but some patients do not develop clinical
symptoms until they are older[3]. The most common symptoms are anxiety,
lethargy and apathy while intrahepatic portosystemic shunts and
cirrhosis cause hepatic encephalopathy more commonly[4,5].
Ultrasonography, magnetic resonance imaging and/or computed tomography
were used for definitive diagnosis [6].
Case History
Two-year-old, male, mix-breed dog presented with an
epileptic seizures and suspicion of foreign body ingestion. Anamnesis
revealed that he had abnormal activities such as allotriophagia and
increased aggression for the last four months. Body temperature,
respiratory and pulse rate were in the normal range but there was
abdominal discomfort during palpation. While the CBC’s results were
within normal ranges, serum ALT, AST and ALP levels were doubled. The
serum ammonium level (SAL) was high (376 mmol/L).Urinalysis revealed
proteinuria (2+) and bilirubinuria (2+), significant amount of ammonium
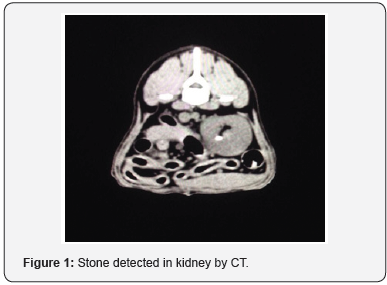
biurate crystals were present in the urinary sediment. CT revealed
multiple foreign bodies in the stomach stones in the bladder and both
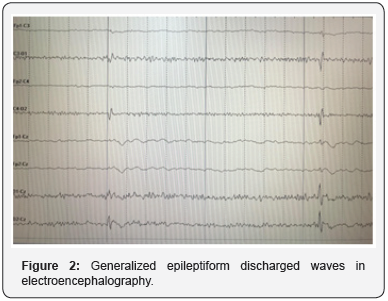
kidneys (Figure1). Generalized epileptiform waves were observed in
electroencephalography (Figure 2).According to our findings, diagnosis
of portosystemic shunt was made, and an operation was planned in order
to correct it surgically.
Supporting therapy was begun immediately after the
operation. Lactulose (5mls per 2.5 lbs. qid) was used for binding
the ammonia present in the intestines. Phenobarbital (2mg/kg
Bid) was given to inhibit the tonic-clonic epileptic seizures. After
the operation SAL was decreased rapidly to 122 mmol/L. But the
patient died three months after the operation. During the post
mortem examination; stones of 4 mm diameter were detected
in the kidneys and in the urinary bladder. There was also micro
hepatica, portal fibrosis, thyroid gland degeneration and chronic
interstitial nephritis.
Discussion
Porto-systemic encephalopathy is a reversible, complex
neuropsychiatric syndrome characterized by disturbances in
consciousness and behavior, personality changes and fluctuating
neurological signs and distinctive electroencephalographic
changes, which occur secondary to chronic liver disease[7,8].
Operative ligation of portosystemic shunts is effective in
controlling chronic portosystemic encephalopathy, but also
holds a high mortality rate[9,10]. In our patient presenting
with high SAL and tonic-clonic seizures, we suspected presence
of a portosystemic shunt. Surgery revealed an extrahepatic
portosystemic shunt and it was corrected. However, the results
were not satisfying; ammonium levels have started to rise
again a month after the procedure and even leaded to more
severe symptoms. We believe that there was also intrahepatic
microvascular dysplasia. Quality of life was deteriorated day-byday
and patient was euthanized in accordance with the request
by care-givers three months after the surgery.
Conclusion
Surgical correction of the portosystemic shunt may
provide a cure for extra-hepatic portosystemic shunt induced
encephalopathy, but success of treatment is low in the presence
of portal vein hypoplasia, microvascular intrahepatic shunt or
cirrhosis.
To know more about journal of veterinary science impact factor: https://juniperpublishers.com/jdvs/index.php
To know more about Open Access Publishers: Juniper Publishers




Comments
Post a Comment